Eyelid & Orbital Trauma - Anatomy
Our eyes are probably the most important vital structures we have in our body. They discovered on the surface by a thin layer of skin and soft tissue called the eyelids. The eyelids serve multiple purposes including protecting the eyeball from injury, controlling the amount of light that enters the eye and also constantly lubricating the eyeball with tears secreted by the lacrimal gland during blinking. All these functions together help maintain the structural integrity of the eyeball and protect them from external influences.
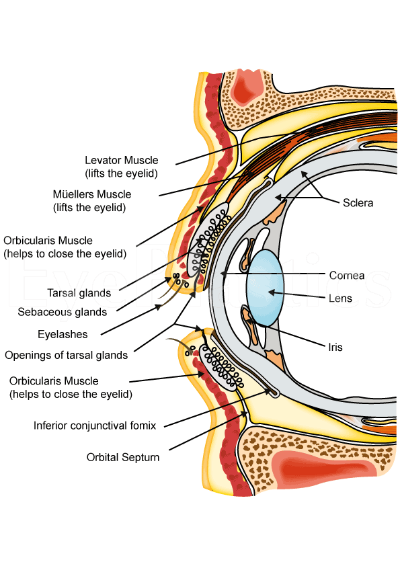
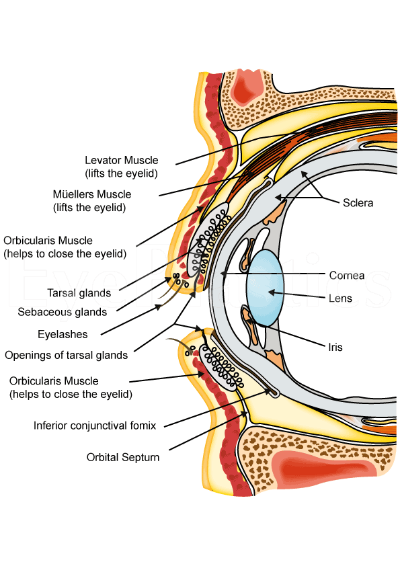
From an anatomical point of view, the eyelid consists primarily of skin, underlying soft tissue also called a subcutaneous tissue and a thin layer of muscle called the orbicularis oculi. Under this muscle are other issues that divide the area into different planes. These are called septum and include the fibrous orbital septum and tarsi. In adds to to this, in order for the eyelids to open are lid retractors that help assist blinking. Finally, there also exists a small amount of fat tissue as well. The eyeball is covered by a thin layer of tissue called the conjunctiva.
Anatomy of the eyelid
The description above only offers a superficial overview of the anatomy of the eyelid. If one were to look at the eyelid in a more detailed manner, a sagittal section taken across the eyelid will offer a clear view of the various structures that form it. Of course, it must be borne in mind that the structures that are visualised depend on the plane at which the sections are taken.
As mentioned above, the tissues can be divided into planes by structures called the septum. The orbital septum differentiates the orbital tissue from the lid. Behind the septum are a number of different other structures, a knowledge of which is essential if surgery is to be performed. In particular, it is essential to identify the anterior and posterior lamellae. In essence, the anterior lamella consists of the skin and the orbicularis oculi muscle while the posterior lamella consists of the conjunctiva and the tarsus.
Let's take a look at the structures of the eyelid in a bit more detail.
Layers & Components of the Eyelid
Skin
- thinnest in body, no subcutanous fat
- upper lid crease (fold) = levator . attachment to pretarsal orbicularis and skin; located at level of sup border of tarsus
- upper puntca is more medial
- mucocutaneous border is post to meibomian gland level
- gray line = muscle of Riolan (superficial orbicularis)
- Zeis, sebaceous glands (holocrine) with cilia
- Moll glands (only apocrine gland on lid) with skin
- 100 lashes on upper lid, 50 on lower
Blood supply
- extensive anastamosis between supraorbital, lacrimal branches of ophthalmic a. (from internal carotid) and angular and temporal a. (from ext carotid)
- venous drainage: pretarsal, poatarsal
- NO lymphatics for the orbit except in conjunctiva
- eyelid medial lymphatics drain to submandibular nodes and laterally to preauricular nodes
Subcutaneous tissue
- no fat, loose connective tissue holds fluid in preseptal > pretarsal area b/c less firmly attached
Orbicularis Muscle
- main protractor
- supplied by Cranial Nerve VII, narrows PF, helps lacrimal pumporbital
- voluntary sphincter (wink, blepharospasm)
- origin at medial canthal tendon and corrugator supercilius muscle
- palpebral (pretarsal & preseptal)
- reflex blink and involuntary
- pretarsal origin at post lacrimal crest (most important to keep lid apposed to globe to let punctum lie in tear lake ) & ant limb of med canthal tendon; deep head of pretarsal m. (Horner’s tensor tarsi) encircles canaliculi to facilitate tear drainage
- upper & lower segments of pretarsal orb m. fuse to become lateral canthal tendon
- pretarsal muscle firmly adherent
- pretarsal muscle of Riolan = gray line = superficial orbicularis
- Septum
- extension of periosteum
- in non-Asians, upper lid septum fuses w/levator aponeurosis. 2-5 mm above sup tarsal border; in lower lid it fuses w/capsulopalpebral fascia at or just below inf tarsal border
- passes medially in front of trochlea
- barrier to hemorrhage and infection between lid and orbit
- orb fat can herniate through septum into lids causing bags
- central orb fat pad lies behind septum, in front of levator aponeurosis.
- Tarus
- dense connective tissue, attach med & lat to periosteum
- 1 x 29 x 11 mm upper lids, 4 mm vertical height in lower lids
- meibomian glands are modified holocrine glands
- in upper lid marginal arcade lies 2 mm sup to lid margin, ant to tarsus
- peripheral art arcade is sup to tarsus, between levator aponeurosis, Muller’s
- Conjunctiva
- mucin is produced from goblet cells
- aqueous is produced from glands of l Krause & Wolfring
- Eyelid Retractors (muscle)
- Upper lid
- Levator Palpebrae Superioris
- starts just above annulus of Zinn, then 40 mm of muscle, then 14-20 mm of aponeurosis.
- becomes vertical near Whitnall's (superotransverse) ligament (near transition m. to aponeurosis.) which is a fulcrum for vertical lid retraction (lower lid analog is Lockwood’s ligament)
- Whitnall's ligament is condensation of tissue around SR and LPS, helps suspend tissue
- levator aponeurosis: attaches to lower 1/2 of ant tarsus; lat horn of aponeurosis divides lacrimal gland into orb and palpebral lobes, attaches to lat orb tubercle; medial horn attaches to post lacrimal crest
- lid crease is formed by attachment of ant portion of aponeurosis w/ septum between the pretarsal orbicular m.’s: here the pretarsal tissues are in close apposition to underlying tarsus
- Superior Tarsal Muscle of Muller
- posterior to LPS
- sympathetically innervated; use neo drops to test function in Ptosis w/u: normal = 2 mm lift
- origin from under LPS, attaches to upper tarsus, firm attachment to conj
- Lower Eyelids
- Inferior Tarsal muscle
-
-
- Capsulopalpebral Fascia
- lower lid analog to levator aponeurosis
- originates from attachments to Inferior rectus ; therefore do vertical m. surgery before lid surgery
- inserts onto lower tarsal border
- inferior tarsal m. is analog to Muller’s, runs post to Capsulopalpebral Fascia
.jpg)